Strengthening Adolescent Health through Community-Led Digital Interventions
Last updated on: May 02, 2025 by Avni Team
Introduction
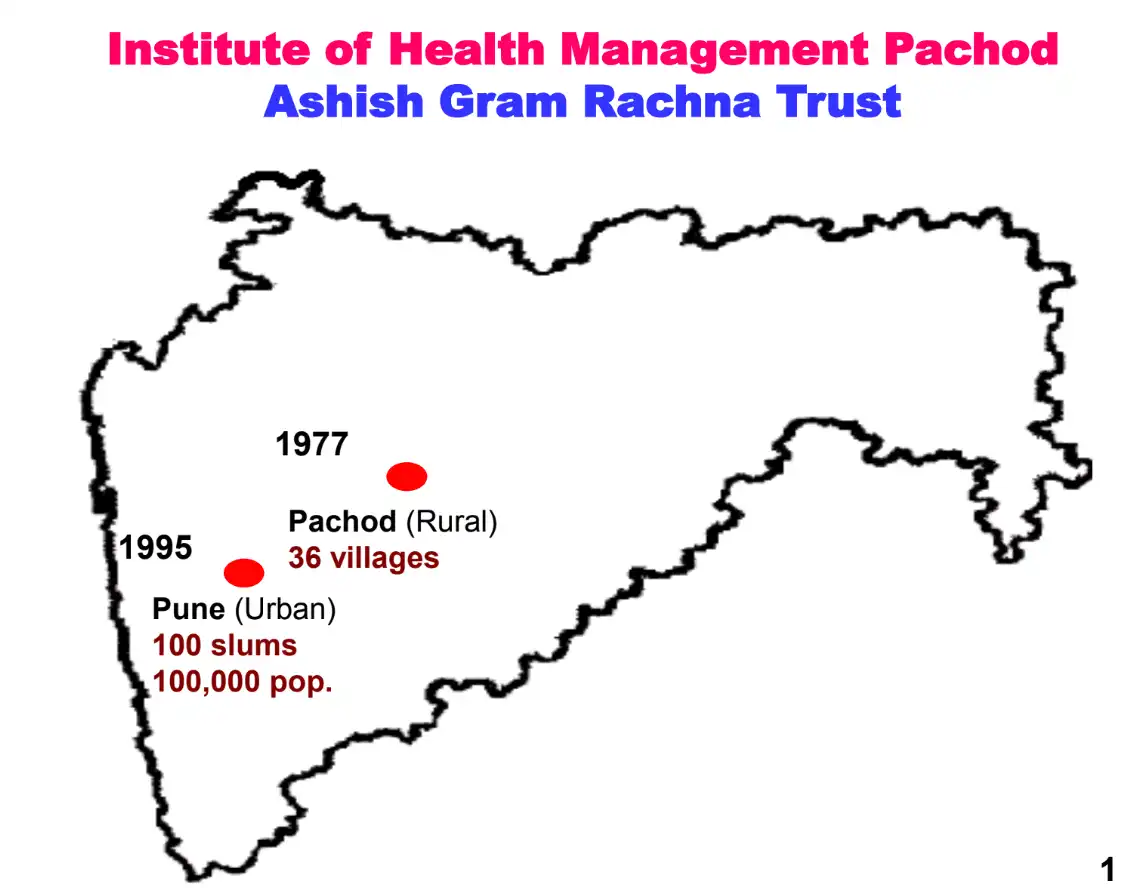
Over the last 45 years, the Institute of Health Management Pachod (IHMP) – a non-profit organisation – has been at the forefront of addressing critical public health issues faced by disadvantaged communities in India. Since its establishment in 1979, IHMP has positively impacted over seven million people, focusing on maternal and neonatal health, child health, sexual and reproductive health, family planning, and adolescent health and development.
A major focus over the last 25 years has been on safeguarding and transforming the lives of vulnerable adolescent girls in rural and urban slum communities.
IHMP has provided life skills education to 103,000 unmarried girls, delaying marriage age from 14.5 to 18 years, while also engaging 8,600 boys and young men to prevent child marriage and promote gender-equitable behaviours.
The Life skills Education for adolescent girls was scaled up through a network of 7 NGOs with equally encouraging results similar to the pilot project.
IHMP’s sexual and reproductive health interventions have reached over 127,000 married adolescent girls, significantly increasing contraceptive use, delaying first pregnancies, and reducing maternal, neonatal and child morbidity and mortality.
Problem Statement & Intervention 1: Addressing Health Risks Among Adolescent Girls
The villages of central Maharashtra and the urban slums of Pune presented several public health challenges:
- High Health Risks: Early pregnancies led to increased adolescent deaths and maternal and neonatal morbidity.
- Limited Access to Services: Adolescent girls and young women had limited access to sexual and reproductive health services.
- Behavioral Barriers: Lack of awareness had a major influence on health seeking and utilisation behaviours and effective use of healthcare facilities.
IHMP’s Integrated Reproductive and Sexual Health and Family Planning Project focused on:
- Providing life skills education with the aim of empowering adolescent girls in order to prevent early marriages.
- Increasing family planning awareness
- Improving access to contraceptives to delay early pregnancy and for adequate spacing between pregnancies
- Improving access to antenatal and home based postnatal and neonatal care services.
- Identifying girls and young women with danger signs and linking them to appropriate secondary or tertiary health care services
- Engaging and educating boys and young men in order to prevent child marriage and influence their attitudes and gender inequitable behaviours, including intimate partner violence.
The intervention relied on a community-based model, led by ASHA workers through regular home visits, paper-based registers, and monthly micro-plans. This manual model laid a strong foundation for scaling up.
The interventions were scaled through a network of NGOs in 120 villages in 5 of the most backward districts of Maharashtra. The impact of the interventions were reported in The Lancet as follows:
Efficacy of an intervention for improving the reproductive and sexual health of married adolescent girls and addressing the adverse consequences of early motherhood
Findings:
- Baseline comparability:
Respondents from intervention and control sites were similar at the start for most key indicators. -
Age at first birth:
- Median age at first birth at intervention sites rose from 16.9 years (2008) to 18.1 years (2010).
-
Contraceptive use:
- Intervention: 33.7%
- Control: 6.4%
- (OR 7.45, 95% CI 5–11)
-
Early antenatal registration:
- Intervention: 78.7%
- Control: 54.7%
- (OR 2.93, 95% CI 2.11–4.06)
-
Minimum standard antenatal care received:
- Intervention: 56.1%
- Control: 24.3%
- (OR 3.89, 95% CI 2.78–5.48)
-
Treatment for antenatal complications:
- Intervention: 87.6%
- Control: 77.1%
- (OR 2.18, 95% CI 1.21–3.12)
-
Treatment for postnatal/neonatal complications:
- Intervention: 78.8%
- Control: 62.0%
- (p = 0.07; marginal significance)
-
Treatment for reproductive tract/sexually transmitted infections (RTI/STI):
- Intervention: 60.4%
- Control: 28.9%
- (OR 3.76, 95% CI 2.34–6.05)
-
HIV testing:
- Intervention sites: Increased from 11.7% (2008) to 58.7% (2010)
- Control sites: Increased from 1.8% (2008) to 15.9% (2010)
Interpretation: Focused, community based interventions, implemented by frontline health workers result in a rapid and significant improvement in utilization and coverage with reproductive health services among married adolescent girls. The interventions were implemented primarily through community health workers and auxiliary nurse midwives. With more than 900 000 community health workers and 140 000 auxiliary nurse midwives providing primary level care in India, replication of this strategy seems imminently feasible.
Eventually the intervention was successfully scaled up through 7 primary health centres, in one block, exclusively through the Government health delivery system
Problem Statement & Intervention 2: Improving Efficiency in Healthcare Delivery Through Digital Tools
Despite successful interventions, service delivery inefficiencies emerged:
- Manual Paperwork: Led to frequent human errors, missed visits, and delayed interventions.
- Frontline Worker Burden: Excessive paperwork left less time for community engagement and service provision.
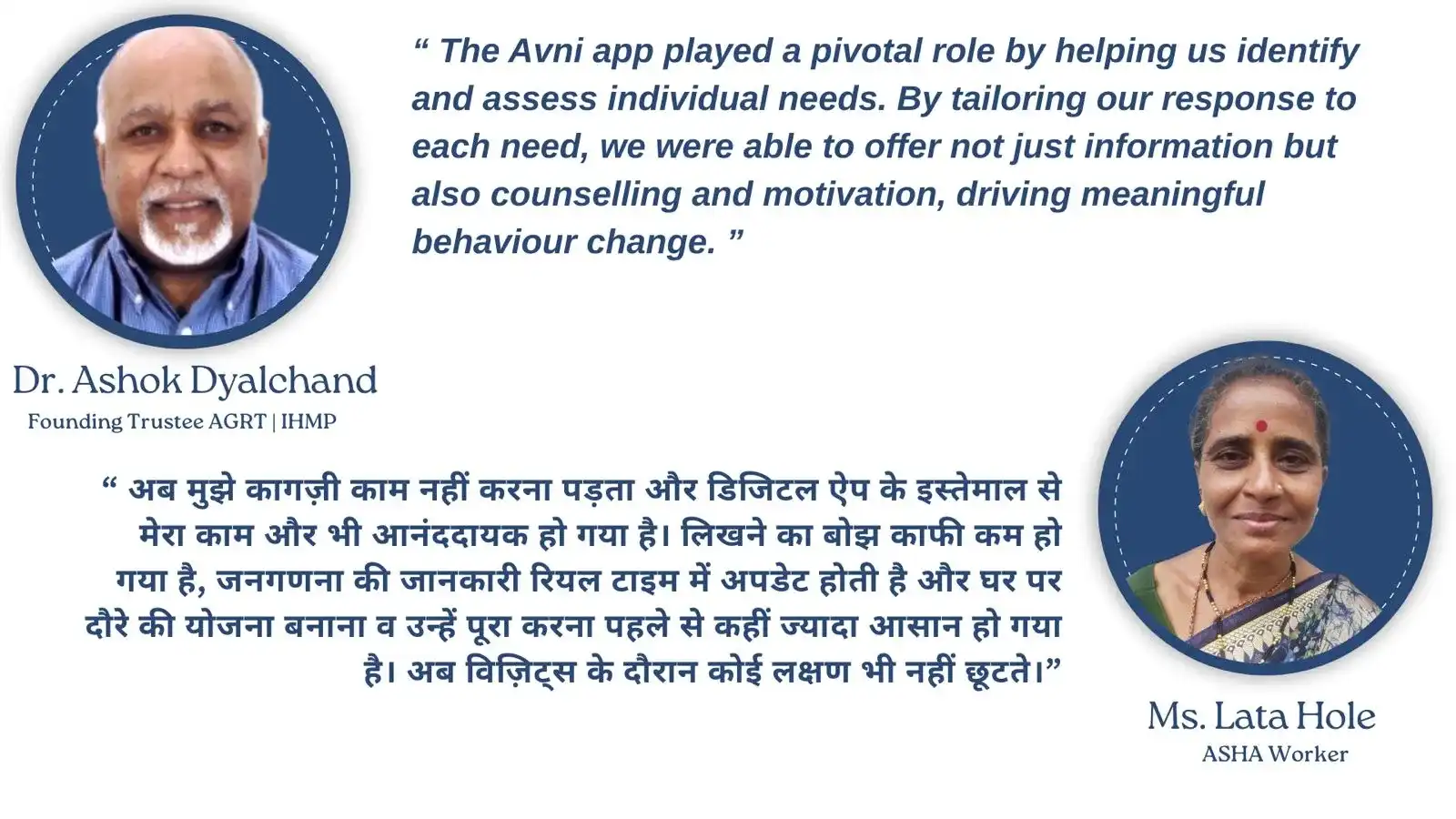
To overcome these, IHMP adopted the Avni platform, digitizing healthcare delivery across urban slums and rural villages.
Key features of the Avni app:
- Census and target population listing: leads to denominator based strategic planning
- Monthly Visit Scheduling and Micro-Planning: Automated schedules based on real-time health assessments, prioritizing high-risk cases.
- Real-time Monitoring: Supervisors track field activities instantly, identifying and addressing gaps.
- Job Aid for ASHAs: The app supports symptom assessments and action guidance during visits.
- Counseling: It facilitates real-time need specific behaviour change communication, counselling and motivation.
- Referrals: The App facilitates timely identification of danger signs and morbidity leading to efficient referral, and supports effective linkage to health services.

Impact and Outcomes
The digital intervention led to significant improvements:
- Behavioral Changes: Increased maternal service utilization and contraceptive use.
- Performance of health workers: Frontline workers demonstrated effective use of the digital App. There was a measurable improvement in the performance of frontline health workers
- Quantitative Gains: From 2021–2024, YMW (young married women) monthly visit coverage rose by 21.4 percentage points.
- Health Status changes: There was a significant reduction in the burden of morbidity and maternal complications.
- Efficiency Gains: ASHA workers reported higher job satisfaction, reduced paperwork, and better income through performance-based incentives.
- Monitoring and Coverage: Real-time data allowed timely corrective actions, improving service coverage.
📹Case Study: IHMP | Digitising Health Programs for Adolescent Girls
Click here to watch the video!
Conclusion
IHMP’s work in Maharashtra’s Marathwada region and Pune’s urban slums shows how digital tools like the Avni app can strengthen public health interventions. By enabling early identification of health needs, real-time monitoring, and effective counselling, the project has improved health outcomes for adolescent girls and young women in vulnerable communities.
The model IHMP has developed is highly replicable and scalable—both in terms of its community-based strategy and the digital infrastructure powered by Avni.
If you're interested in adopting a similar approach or want to learn more about how the Avni platform can support your initiatives:
Let’s work together to scale impactful solutions for better health outcomes.